You find an unresponsive pt. who is not breathing. After activating the emergency response system, you determine there is no pulse. What is your next action?
Start chest compressions of at least 100 per min.
You are evaluating a 58-year-old man with chest pain. The blood pressure is 92/50 mm Hg, the heart rate is 92/min, the nonlabored respiratory rate is 14 breaths/min, and the pulse oximetry reading is 97%. What assessment step is most important now?
Obtaining a 12 lead ECG.
What is the preferred method of access for epi administration during cardiac arrest in most pts?
Peripheral IV
An AED does not promptly analyze a rythm. What is your next step?
Begin chest compressions.

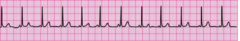
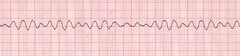
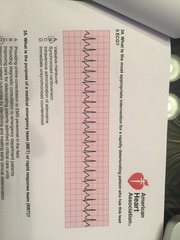
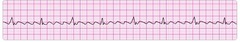
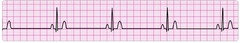
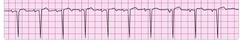
You have completed 2 minutes of CPR. The ECG monitor displays the lead II rhythm below, and the patient has no pulse. Another member of your team resumes chest compressions, and an IV is in place. What management step is your next priority?
Administer 1mg of epinephrine
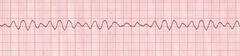
During a pause in CPR, you see this lead II ECG rhythm on the monitor. The patient has no pulse. What is the next action?
Resume compressions
What is a common but sometimes fatal mistake in cardiac arrest management?
Prolonged interruptions in chest compressions.
Which action is a componant of high-quality chest comressions?
Allowing complete chest recoil
Which action increases the chance of successful conversion of ventricular fibrillation?
Providing quality compressions immediately before a defibrillation attempt.
Which situation BEST describes pulseless electrical activity?
Sinus rythm without a pulse
What is the BEST strategy for performing high-quality CPR on a patient with an advanced airway in place?
Provide continuous chest compressions without pauses and 10 ventilations per minute.
Three minutes after witnessing a cardiac arrest, one member of your team inserts an endotracheal tube while another performs continuous chest compressions. During subsequent ventilation, you notice the presence of a waveform on the capnography screen and a PETCO2 level of 8 mm Hg. What is the significance of this finding?
Chest compressions may not be effective.
The use of quantitative capnography in intubated patients
allows for monitoring of CPR quality.
For the past 25 minutes, an EMS crew has attempted resuscitation of a patient who originally presented in ventricular fibrillation. After the first shock, the ECG screen displayed asystole, which has persisted despite 2 doses of epinephrine, a fluid bolus, and high-quality CPR. What is your next treatment?
Consider terminating resuscitive efforts after consulting medical control.
Which is a safe and effective practice within the defibrillation sequence?
Be sure oxygen is not blowing over the patient's chest during the shock.
During your assessment, your patient suddenly loses consciousness. After calling for help and determining that the patient is not breathing, you are unsure whether the patient has a pulse. What is your next action?
Begin chest compressions.
What is an advantage of using hands-free defibrillation pads instead of defibrillation paddles?
Hands-free pads allow for a more rapid defibrillation.
What action is recommended to help minimize interruptions in chest compressions during CPR?
Continue CPR while charging the defibrillator.
Which action is included in the BLS survey?
Early defibrillation
Which drug and dose are recommended for the management of a patient in refractory ventricular fibrillation?
Amioderone 300mg
What is the appropriate interval for an interruption in chest compressions?
10 seconds or less
Which of the following is a sign of effective CPR?
PETCO2 ≥10 mm Hg
What is the primary purpose of a medical emergency team (MET) or rapid response team (RRT)?
Identifying and treating early clinical deterioration.
Which action improves the quality of chest compressions delivered during a resuscitation attempt?
Switch providers about every 2 minutes or every 5 compression cycles.
What is the appropriate ventilation strategy for an adult in respiratory arrest with a pulse rate of 80/min?
1 breath every 5-6 seconds
A patient presents to the emergency department with new onset of dizziness and fatigue. On examination, the patient's heart rate is 35/min, the blood pressure is 70/50 mm Hg, the respiratory rate is 22 breaths/min, and the oxygen saturation is 95%. What is the appropriate first medication?
Atropine 0.5mg
A patient with dizziness and shortness of breath with a sinus bradycardia of 40/min. The initial atropine dose was ineffective, and your monitor/defibrillator is not equipped with a transcutaneous pacemaker. What is the appropriate dose of dopamine for this patient?
2 to 10 mcg/kg per minute
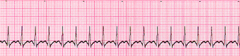
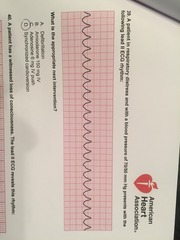
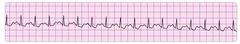
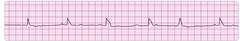
A patient has sudden onset of dizziness. The patient's heart rate is 180/min, blood pressure is 110/70 mm Hg, respiratory rate is 18 breaths/min, and pulse oximetry reading is 98% on room air. The lead II ECG is shown below:
Vagal manuever.
A monitored patient in the ICU developed a sudden onset of narrow-complex tachycardia at a rate of 220/min. The patient's blood pressure is 128/58 mm Hg, the PETCO2 is 38 mm Hg, and the pulse oximetry reading is 98%. There is vascular access at the left internal jugular vein, and the patient has not been given any vasoactive drugs. A 12-lead ECG confirms a supraventricular tachycardia with no evidence of ischemia or infarction. The heart rate has not responded to vagal maneuvers. What is the next recommended intervention?
Adenosine 6mg IV push
You are receiving a radio report from an EMS team en route with a patient who may be having an acute stroke. The hospital CT scanner is not working at this time. What should you do in this situation?
Divert the patient to a hospital 15 minutes away with CT capabilities.
Choose an appropriate indication to stop or withhold resuscitative efforts.
Evidence of rigor mortis.
A 49-year-old woman arrives in the emergency department with persistent epigastric pain. She had been taking oral antacids for the past 6 hours because she thought she had heartburn. The initial blood pressure is 118/72 mm Hg, the heart rate is 92/min and regular, the nonlabored respiratory rate is 14 breaths/min, and the pulse oximetry reading is 96%. Which is the most appropriate intervention to perform next?
Obtain a 12 lead ECG.
A patient in respiratory failure becomes apneic but continues to have a strong pulse. The heart rate is dropping rapidly and now shows a sinus bradycardia at a rate of 30/min. What intervention has the highest priority?
Simple airway manuevers and assisted ventilations.
What is the appropriate procedure for endotracheal tube suctioning after the appropriate catheter is selected?
Suction during withdrawal but for no longer than 10 seconds.
While treating a patient with dizziness, a blood pressure of 68/30 mm Hg, and cool, clammy skin, you see this lead II ECG rhythm:What is the first intervention ?
Atropine 0.5mg
A 68-year-old woman experienced a sudden onset of right arm weakness. EMS personnel measure a blood pressure of 140/90 mm Hg, a heart rate of 78/min, a nonlabored respiratory rate of 14 breaths/min, and a pulse oximetry reading of 97%. The lead II ECG displays sinus rhythm. What is the most appropriate action for the EMS team to perform next?
Cincinnati Prehospital Stroke Scale assessment
EMS is transporting a patient with a positive prehospital stroke assessment. Upon arrival in the emergency department, the initial blood pressure is 138/78 mm Hg, the pulse rate is 80/min, the respiratory rate is 12 breaths/min, and the pulse oximetry reading is 95% on room air. The lead II ECG displays sinus rhythm. The blood glucose level is within normal limits. What intervention should you perform next?
Head CT scan
What is the proper ventilation rate for a patient in cardiac arrest who has an advanced airway in place?
8-10 breaths per minute
A 62-year-old man in the emergency department says that his heart is beating fast. He says he has no chest pain or shortness of breath. The blood pressure is 142/98 mm Hg, the pulse is 200/min, the respiratory rate is 14 breaths/min, and pulse oximetry is 95% on room air. What intervention should you perform next?
Obtain a 12 lead ECG.
You are evaluating a 48-year-old man with crushing substernal chest pain. The patient is pale, diaphoretic, cool to the touch, and slow to respond to your questions. The blood pressure is 58/32 mm Hg, the heart rate is 190/min, the respiratory rate is 18 breaths/min, and the pulse oximeter is unable to obtain a reading because there is no radial pulse. The lead II ECG displays a regular wide-complex tachycardia. What intervention should you perform next?
Synchronized cardioversion
What is the initial priority for an unconscious patient with any tachycardia on the monitor?
Determine whether pulses are present.
Which rhythm requires synchronized cardioversion?
Unstable supraventricular tachycardia
What is the recommended second dose of adenosine for patients in refractory but stable narrow-complex tachycardia?
12mg
What is the usual post-cardiac arrest target range for PETCO2 when ventilating a patient who achieves return of spontaneous circulation (ROSC)?
35-40mm Hg
Which condition is a contraindication to therapeutic hypothermia during the post-cardiac arrest period for patients who achieve return of spontaneous circulation ROSC?
Responding to verbal commands
What is the potential danger of using ties that pass circumferentially around the patient's neck when securing an advanced airway?
Obstruction of venous return from the brain
What is the most reliable method of confirming and monitoring correct placement of an endotracheal tube?
Continuous waveform capnography
hat is the recommended IV fluid (normal saline or Ringer's lactate) bolus dose for a patient who achieves ROSC but is hypotensive during the post-cardiac arrest period?
1 to 2 Liters
What is the minimum systolic blood pressure one should attempt to achieve with fluid, inotropic, or vasopressor administration in a hypotensive post-cardiac arrest patient who achieves ROSC?
90mm Hg
What is the first treatment priority for a patient who achieves ROSC?
Optimizing ventilation and oxygenation.
What should be done to minimize interruptions in chest compressions during CPR?
Continue CPR while the defibrillator is charging.
Which condition is an indication to stop or withhold resuscitative efforts?
Safety threat to providers
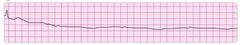
After verifying the absence of a pulse, you initiate CPR with adequate bag-mask ventilation. The patient's lead II ECG appears below. What is your next action?
IV or IO access
After verifying unresponsiveness and abnormal breathing, you activate the emergency response team. What is your next action?
Check for a pulse.
What is the recommendation on the use of cricoid pressure to prevent aspiration during cardiac arrest?
Not recommended for routine use
What survival advantages does CPR provide to a patient in ventricular fibrillation?
Produces a small amount of blood flow to the heart
What is the recommended compression rate for performing CPR?
At least 100 per minute
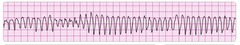
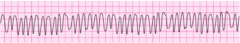
EMS personnel arrive to find a patient in cardiac arrest. Bystanders are performing CPR. After attaching a cardiac monitor, the responder observes the following rhythm strip. What is the most important early intervention?
defibrillation
A patient remains in ventricular fibrillation despite 1 shock and 2 minutes of continuous CPR. The next intervention is to
administer a second shock.
What is the recommended next step after a defibrillation attempt?
Begin CPR, starting with chest compressions.
Which of the following is the recommended first choice for establishing intravenous access during the attempted resuscitation of a patient in cardiac arrest?
Antecubital vein
Which finding is a sign of ineffective CPR?
PETCO2 <10 mm Hg
How often should the team leader switch chest compressors during a resuscitation attempt?
. Every 2 minutes
IV/IO drug administration during CPR should be
given rapidly during compressions
What is the recommended first intravenous dose of amiodarone for a patient with refractory ventricular fibrillation?
300 mg
A team leader orders 1 mg of epinephrine, and a team member verbally acknowledges when the medication is administered. What element of effective resuscitation team dynamics does this represent?
Closed-loop communication
How long should it take to perform a pulse check during the BLS Survey?
5 to 10 seconds
Your rescue team arrives to find a 59-year-old man lying on the kitchen floor. You determine that he is unresponsive and notice that he is taking agonal breaths. What is the next step in your assessment and management of this patient?
Check the patient's pulse.
An AED advises a shock for a pulseless patient lying in snow. What is the next action?
Administer the shock immediately and continue as directed by the AED.
Which treatment or medication is appropriate for the treatment of a patient in asystole?
Epinephrine
What is the minimum depth of chest compressions for an adult in cardiac arrest?
2 inches
A patient with pulseless ventricular tachycardia is defibrillated. What is the next action?
Start chest compressions at a rate of at least 100/min.
You have completed your first 2-minute period of CPR. You see an organized, nonshockable rhythm on the ECG monitor. What is the next action?
Have a team member attempt to palpate a carotid pulse.
Emergency medical responders are unable to obtain a peripheral IV for a patient in cardiac arrest. What is the next most preferred route for drug administration?
Intraosseous (IO)
What is the appropriate rate of chest compressions for an adult in cardiac arrest?
At least 100/min
You are receiving a radio report from an EMS team en route with a patient who may be having an acute stroke. The hospital CT scanner is not working at this time. What should you do in this situation?
Divert the patient to a hospital 15 minutes away with CT capabilities.
A 53-year-old man has shortness of breath, chest discomfort, and weakness. The patient's blood pressure is 102/59 mm Hg, the heart rate is 230/min, the respiratory rate is 16 breaths/min, and the pulse oximetry reading is 96%. The lead II ECG is displayed below. A patent peripheral IV is in place. What is the next action?
Vagal maneuvers
A 49-year-old man has retrosternal chest pain radiating into the left arm. The patient is diaphoretic, with associated shortness of breath. The blood pressure is 130/88 mm Hg, the heart rate is 110/min, the respiratory rate is 22 breaths/min, and the pulse oximetry value is 95%. The patient's 12-lead ECG shows ST-segment elevation in the anterior leads. First responders administered 160 mg of aspirin, and there is a patent peripheral IV. The pain is described as an 8 on a scale of 1 to 10 and is unrelieved after 3 doses of nitroglycerin. What is the next action?
Administer 2 to 4 mg of morphine by slow IV bolus.
A 56-year-old man reports that he has palpitations but not chest pain or difficulty breathing. The blood pressure is 132/68 mm Hg, the pulse is 130/min and regular, the respiratory rate is 12 breaths/min, and the pulse oximetry reading is 95%. The lead II ECG displays a wide-complex tachycardia. What is the next action after establishing an IV and obtaining a 12-lead ECG?
Seeking expert consultation
A postoperative patient in the ICU reports new chest pain. What actions have the highest priority?
Obtain a 12-lead ECG and administer aspirin if not contraindicated.
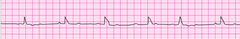
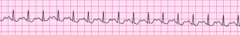
An 80-year-old woman presents to the emergency department with dizziness. She now states she is asymptomatic after walking around. Her blood pressure is 102/72 mm Hg. She is alert and oriented. Her lead II ECG is below. After you start an IV, what is the next action?
Conduct a problem-focused history and physical examination.
What is the recommended oral dose of aspirin for patients suspected of having one of the acute coronary syndromes?
160 to 325 mg

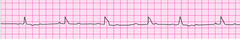
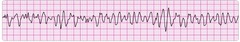
A responder is caring for a patient with a history of congestive heart failure. The patient is experiencing shortness of breath, a blood pressure of 68/50 mm Hg, and a heart rate of 190/min. The patient's lead II ECG is displayed below.
stable supraventricular tachycardia
What is the most appropriate intervention for a rapidly deteriorating patient who has this lead II ECG?
Synchronized cardioversion
What is the purpose of a medical emergency team (MET) or rapid response team (RRT)?
Improving patient outcomes by identifying and treating early clinical deterioration
What is the recommended assisted ventilation rate for patients in respiratory arrest with a perfusing rhythm?
10 to 12 breaths per minute
Family members found a 45-year-old woman unresponsive in bed. The patient is unconscious and in respiratory arrest. What is the recommended initial airway management technique?
Performing a head tilt-chin lift maneuver
A patient in respiratory distress and with a blood pressure of 70/50 mm Hg presents with the following lead II ECG rhythm:
What is the appropriate next intervention?
Synchronized cardioversion
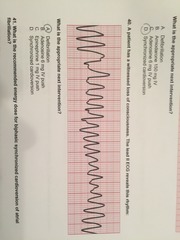
A patient has a witnessed loss of consciousness. The lead II ECG reveals this rhythm:
What is the appropriate next intervention?
Defibrillation
What is the recommended energy dose for biphasic synchronized cardioversion of atrial fibrillation?
120to200J
Which of the following is an acceptable method of selecting an appropriately sized oropharyngeal airway (OPA)?
Measure from the corner of the mouth to the angle of the mandible.
Which is a contraindication to nitroglycerin administration in the management of acute coronary syndromes?
Right ventricular infarction and dysfunction
What is the recommended initial intervention for managing hypotension in the immediate period after return of spontaneous circulation (ROSC)?
Administration of IV or IO fluid bolus
Which is an appropriate and important intervention to perform for a patient who achieves ROSC during an out-of-hospital resuscitation?
Transport the patient to a facility capable of performing PCI.
What is the immediate danger of excessive ventilation during the post-cardiac arrest period for patients who achieve ROSC?
Decreased cerebral blood flow
What is the recommended target temperature range for achieving therapeutic hypothermia after cardiac arrest?
32°C to 34°C
What is the recommended duration of therapeutic hypothermia after reaching the target temperature?
12 to 24 hours
What is the danger of routinely administering high concentrations of oxygen during the post- cardiac arrest period for patients who achieve ROSC?
Potential oxygen toxicity
What is the recommended dose of epinephrine for the treatment of hypotension in a post- cardiac arrest patient who achieves ROSC?
0.1 to 0.5 mcg/kg per minute IV infusion

You have completed 2 min of CPR. The ECG monitor displays the lead below (PEA) and the patient has no pulse. You partner resumes chest compressions and an IV is in place. What management step is your next priority?
Administer 1mg of epinephrine
A patient is in refractory ventricular fibrillation and has received multiple appropriate defibrillation shocks, epinephrine 1 mg IV twice, and an initial dose of 300 mg amiodarone IV. The patient is intubated. A second dose of amiodarone is now called for. The recommend second dose of amiodarone is ?
150 mg IV push
A patient is in refractory ventricular fibrillation. High CPR is in progress and shocks have been given. One dose of epinephrine was given after the second shock. An anti arrhythmic drug was given immediately after the the third shock. What drug should the team leader request to be prepared for administration next?
second dose of epinephrine 1 mg
A patient is in pulseless ventricular tachycardia. Two shocks and 1 dose of epinephrine has been given. Which is the next drug to anticipate to administer?
amiodarone 300 mg
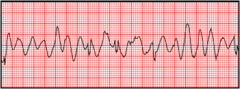
You are monitoring a patient with chest discomfort who suddenly becomes unresponsive. You observe the following rhythm on the cardiac monitor. A defibrillator is present. What is your first action?
Give a single shock
what do you do after return of spontaneous circulation
maintain O2 sat at 94%
treat hypotension (fluids vasopressor)
12 lead EKG
if in coma consider hypothermia
if not in coma and ekg shows STEMI or AMI consider re-perfusion
what are the 5 h's and 5 t's
hypovolemia
hypoxia
hydrogen ion (acidosis)
hypo/hyperkalemia
hypothermia
tension pneumothorax
tamponade, cardiac
toxins
thrombosis, pulmonary
thrombosis, coronary
Bradycardia require treatment when?
chest pain or shortness of breath is present
how do you treat non-symptomatic bradycardia
monitor and observe
what constitutes symptomatic bradycardia
hypotension
altered mental status
signs of shock
chest pain
acute heart failure
A patient with sinus bradycardia and a heart rate of 42 has diaphoresis and blood pressure of 80/60. What is the initial dose of atropine?
0.5 mg
how do you treat symptomatic bradycardia
give 0.5mg atropine every 3-5 mins to max of 3mg
if that doesn't work try one of the following:
transcutaneous pacing
2-10mcg/kg / minute dopamine infusion
2-10mcg per minute epinephrine infusion
what is considered a tachycardia requiring treatment
over 150 per minute
when do you consider cardioversion
if persistent tachycardia is causing:
hypotension
altered mental status
signs of shock
chest pain
acute heart failure
if persistent tachycardia does not present with symptoms what do you need to consider
wide QRS?
greater than 0.12 seconds
Your patient has been intubated. IV/IVO access is not available. Which combination of drugs can be administered by endotracheal route?
Lidocaine, epinephrine, vasopressin

reentry supraventricular tachycardia
polymorphic ventricular tachycardia - aka torsades

atrial fibrilation
sinus tachycardia
coarse ventricular fibrillation
atrial flutter

reentry supraventricular tachycardia
sinus bradycardia

monomorphic ventricular tachycardia
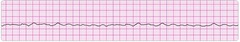
fine ventricular fibrillation

second degree AV block type 1 wenckenbach

second degree AV block mobitz type 2
third degree AV block
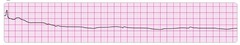
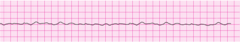
asystole
normal sinus rhythm

pulseless electrical activity
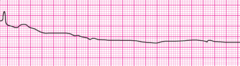
agonal rhythm/asystole
The five links in the adult Chain of Survival
1- Immediate activation of EMS
2- Early CPR
3- Rapid defibrillation (not in peds)
4- Effective advanced life support
5- Integrated post-cardiac arrest care
Type of breaths (not normal) that may be present in the first minutes after sudden cardiac arrest
Agonal gasps
To place the pads on the victims bare chest, Place one pad on the upper-right chest (below the collarbone) and place the other pad
to the side of the left nipple, with the top edge of the pad a few inches below the armpit
If the heart muscle resets and initiates an organized rhythm this is called
ROSC return of spontaneous circulation
a patient is in cardiac arrest. ventricular fibrillation has been refractory to an initial shock. if no pathway for medication is in place, preferred method?
IV or IO
A patient has sinus bradycardia with a heart rate of 36/min. Atropine has been administered to a total dose of 3 mg. A transcutaneous pacemaker has failed to capture. The patient is confused, and her blood pressure is 100/60 mm HG. What is now indicated?
EPI 2-10 mcg/min
A patient with ST-segment elevation MI has ongoing chest discomfort. Fibrinolytic therapy has been ordered. Heparin 4000 units IV bolus was administered, and a heparin infusion of 1000 units per hour is being administered. ASA was not taken by the patient because he had a history of gastritis treated 5 years ago. What is the next action?
ASA 160-325 mg chew
A patient has a rapid irregular wide-complex tachycardia. The ventricular rate is 138/min. He is asymptomatic, with a blood pressure of 110/70 mm Hg. He has a history of angina. What should you do?
seek expert consultation
A 35 year old woman has palpitations, light headedness, and a stable tachycardia. The monitor shows a regular narrow-complex QRS at a rate of 180/min. Vagal maneuvers have not been effective in terminating the rhythm. An IV has been established. What drug should be administered?
adenosine 6 mg
A 57 year old woman has palpitations, chest discomfort, and tachycardia. The monitor shows a regular wide-complex QRS at a rate of 180 bpm. She becomes diaphoretic and her blood pressure is 80/60 mm Hg. What is the next action?
cardioversion
when does bradycardia require treatment?
hypotension
You arrive on the scene with the code team. High-quality CPR is in progress. An AED has previously advised "no shock indicated". A rhythm check now finds asystole. After resuming high-quality compressions, your next action is to what?
establish IV or IO access
you are caring for a 66 year old man with a history of a large intracerebral hemorrhage 2 months ago. He is being evaluated for another acute stroke. the ct scan is negative for hemorrhage. The patient is receiving oxygen via nasal cannula at 2 L/min, and an IV has been established. His blood pressure is 180/100 mm Hg. Which drug do you anticipate giving?
aspirin
A 62 year old man suddenly experienced difficulty speaking and left-sided weakness. He was brought into the emergency department. He meets initial criteria for fibrinolytic therapy, and a CT scan of the brain is ordered. What are the guidelines for antiplatelet and fibrinolytic therapy?
hold aspirin for at least 24 hours if rtPA is administered
a 45 year old woman has a history of palpitations develops lightheadedness and palpitations. She has received adenosine 6 mg IV for SVT without conversion. BP 128/70. next step?
adenosine 12 mg
STEMI intervention is most important in reducing patients in hospital and 30 day mortality?
reperfusion therapy
a patient has been resuscitated from cardiac arrest. During post-ROSC treatment, the patient becomes unresponsive, with the rhythm VT. What tx is indicated
unsynchronized high energy shock
which action should you take immediately after providing an AED shock
resume chest compressions
which action causes air to enter victim's stomach (gastric inflation) during bag-mask ventilation
ventilation too quickly,

A patient becomes unresponsive. You are uncertain if a faint pulse is present with the rhythm
below. What is your next action?
CPR
you are the code team leader and arrive to find a patient with CPR in progress. On next rhythm check NSR. Pt reported chest discomfort and then collapsed. She has no pulse or respirations. Bag-mask ventilations are producing visible chest rise and IO access has been established. Intervention?
EPI 1 mg
refractory ventricular fibrillation. 3rd shock just administered. what is next action
resume high-quality chest compression
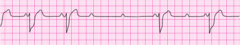
2nd degree mobitz

2nd degree wenckebach
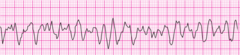
coarse V fib
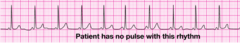
PEA
fine V Fib
A patient was in refractory ventricular fibrillation. A third shock has just been administered. Your
team looks to you for instructions. Your immediate next order is?
resume high quality chest compressions
